ABA Workflows Are Being Put to the Test in 2026
ABA organizations have spent years building efficient scheduling and service delivery workflows. Many platforms were designed around a schedule-first assumption: if a service appears on the calendar, the system treats it as deliverable and eventually billable.
For a long time, this approach worked. Payer enforcement was lighter, and critical safeguards often lived with scheduling teams, billing specialists, or experienced staff who understood payer nuances and caught issues before claims were submitted.
Anthem-affiliated plans implementing new ABA claim requirements effective January 1, 2026 significantly reduce the margin for error.
Now is the right moment to step back and ask a question with major operational consequences:
How Does Your Platform Actually Decide What Can Be Delivered and Billed?
Not what the platform promises. Not what internal policy says. What happens in real-world scenarios when schedules shift, sessions move, and last-minute changes occur?
Schedule-First vs Authorization-Driven: A Practical Framework
Most provider organizations fall somewhere along a spectrum, but operational behavior typically aligns with one of two models.
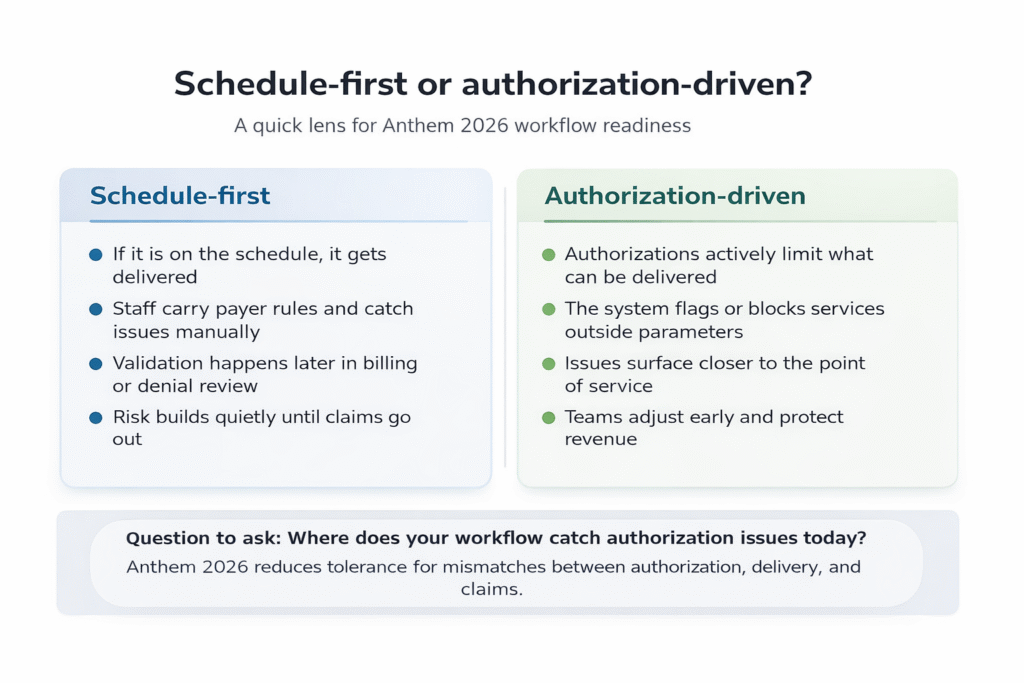
The two operational architectures emerging in ABA.
Schedule-First Behavior
In a schedule-first environment, the calendar drives service delivery. If a session is scheduled, the system allows it to occur.
Compliance depends heavily on staff following payer rules perfectly, every time. Validation usually happens later during billing, denial review, or manual reconciliation.
The risk is rarely obvious in the moment. It builds quietly until claims are submitted, when teams discover:
-
Unit overages
-
Service-context mismatches
-
Documentation gaps
-
Coding inconsistencies
These issues often translate into denials, delayed revenue, and administrative rework.
Authorization-Driven Behavior
In an authorization-driven model, approvals actively constrain what can be delivered.
The system flags or prevents services that fall outside authorized parameters, surfacing risk earlier, closer to care delivery, when teams can still adjust without financial impact.
Many organizations believe they operate this way until they trace a single case from authorization → schedule → delivery → claim.
That exercise often reveals where mismatches are truly detected.
Pro Tip: Trace one real client journey from authorization to claim submission. You may quickly see whether your safeguards are proactive or reactive.
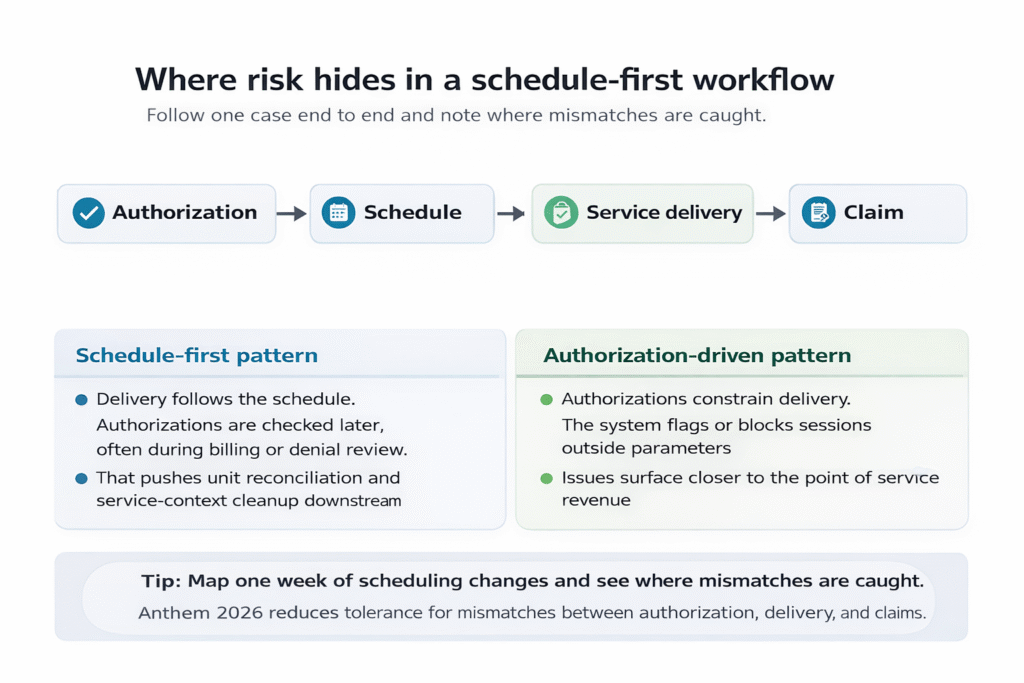
How authorization risk travels downstream when caught too late.
Why Anthem’s 2026 Changes Raise the Stakes
Anthem’s updates reflect a broader shift across commercial payers:
-
Less tolerance for mismatches between authorization, delivery, and billing
-
Tighter enforcement of unit logic
-
Reduced opportunity for retroactive corrections
In this environment, operational pressure typically shows up in three areas:
Units
Was the delivered care aligned with what was approved for that time period?
Documentation and Coding
Does the clinical note support what is being billed?
Downstream Denial Work
Is manual reconciliation becoming routine rather than occasional?
Even high-performing operations teams can feel the impact if their systems do not enforce, or at minimum surface, authorization constraints early.
Center-Based vs Home-Based Care Adds Complexity
Operational realities vary by service model.
Center-based programs benefit from consistency but must manage higher volume and scheduling complexity.
Home-based programs face greater variability, frequent rescheduling, and environmental unpredictability.
Both models can remain compliant. The differentiator is whether your technology and workflows identify authorization conflicts early enough to act before a claim becomes a denial.
Where ATrack Fits In
ATrack is not here to declare a single “correct” architecture.
Our role is to help providers clearly understand how their systems behave day to day, determine whether risk is being managed by people or software, and evaluate whether payer changes introduce new exposure.
When we speak with provider teams, we typically see one of two outcomes:
-
You confirm your controls are strong. That clarity reduces uncertainty and supports confident scaling.
-
You uncover gaps you did not realize existed. Addressing them early is far less costly than reacting to denials or revenue leakage later.
Either outcome replaces assumptions with actionable insight.
Pressure Test Your Workflow Before Payers Do
We invite you to connect with our subject-matter experts for a working session focused on:
-
How Anthem’s 2026 changes interact with your workflows
-
Where your platform sits on the schedule-first vs authorization-driven spectrum
-
What, if anything, should be adjusted to protect revenue
👉 Schedule Your Anthem 2026 Review
This is not a product pitch. It is a collaborative review designed to validate what is already working and identify potential risk areas before they surface downstream.